
When employers consider a referenced-based pricing (RBP) plan, one concern comes up repeatedly: Will my employees be able to see their providers?
It’s a fair question, and one that often reflects broader uncertainty about access and potential disruption.
At Homestead, we believe access shouldn’t be left to chance. That’s why our open access plans include convenient access to more than 700,000 physicians, specialists and ancillary providers through Prime Health Services’ Physician Only Network (PON).
We also help members see the providers they choose through our Clear the Path program, a proactive approach to provider relations designed to remove barriers before members ever need care.
What “Clearing the Path” Actually Means
Clear the Path isn’t reactive. It doesn’t start when a claim is denied or a member is frustrated. Clear the Path is proactive and starts before the plan goes live.
Our Provider Relations team uses historical claims data to identify the providers members already rely on most. We proactively confirm continued access well in advance of the plan’s effective date, allowing potential issues to be identified and resolved early.
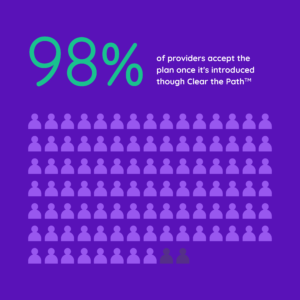
This approach is a key reason Homestead consistently achieves a 98% provider acceptance rate.
How Proactive Provider Outreach Works
Here’s what happens behind the scenes:
- Claims history helps us identify the providers most important to members
- Providers are then grouped based on whether they already participate in Prime’s national network
- For providers outside the network, we then check whether Homestead has prior experience working with them
- If a provider is outside the network and we have limited or no prior experience, our team reaches out directly to explain the plan and confirm how claims will be submitted
- Our team explains the reimbursement approach and confirms the provider’s willingness to accept the plan.
- Once outreach is complete, we communicate back to the employer, and support member communication as needed, so they know the path has been cleared prior to the effective date.
Providers aren’t asked to “figure it out”, they are supported through clear communication.
Questions Brokers & Employers Hear Most
Clear the Path exists because we understand the concerns and we’ve built the process to answer them directly.
Q: What if a large hospital says they don’t accept RBP?
Provider acceptance is rarely a binary yes or no. Our team engages in education, clarifies reimbursement expectations, and explores solutions such as prior experience, alternative facilities, or targeted agreements when appropriate.
Q: What happens if a provider doesn’t accept the first payment?
If questions arise after care is delivered, our team steps in to manage communication, address concerns, and protect the member from disruption.
Q: How do you mitigate balance billing risk?
In the off chance a balance bill happens, Homestead handles outreach, negotiation, and resolution. Members are never left to handle the situation on their own.
Q: Can you do direct contracting if needed?
Yes. In certain circumstances, contracting with anchor facilities can be an option when it supports access and member needs in a specific market.
Why Provider Relations Is the Linchpin of RBP Success
Reference-based pricing works when provider relations are strong. Clear the Path connects strategy to execution, ensuring that pricing models are supported by real conversations, real outreach, and real follow-through. It’s the difference between a plan that looks good on paper and one that works in practice.
For brokers, this means confidence in addressing objections.
For employers, it means reassurance that access remains intact.
For members, it means fewer barriers to care.



